ACL – Sports Medicine
The anterior cruciate ligament or ACL is one of the two main ligaments inside of the knee. It crosses the posterior cruciate ligament or PCL and in doing so makes a “cross” thus giving the term cruciate. The ACL is frequently injured in sporting activities. In 80% of the injuries, the event is a non contact deceleration with a pivoting point. There is usually a sensation of a pop and the knee typically causes the athlete to fall and normally stop the competition. The knee then starts to swell for an hour or two. This swelling is secondary to bleeding from the torn ligament and is typically noted above the knee cap area.  The diagnosis of an ACL tear is usually made by a clinical test called a Lachman exam which tests the integrity of the ACL. MRI scans confirm the diagnosis and help determine if additional injuries have occurred. Surgery is delayed until the knee has recovered a full range of motion and swelling has diminished. There is a seven times increased risk of scar tissue formation when the ACL is reconstructed within the first three weeks of injury. Generally when range of motion normalizes surgery can be safely performed. Females have two to four times the risk of ACL injuries compared to males. The reasons are not exactly clear, but there seems to be a correlation between ACL tears and the varying phases of the menstrual cycle. Females also have stronger and quicker quadriceps firing in relation to their hamstrings compared to their male counterparts. Preseason training that focuses on proprioceptive conditioning plus neuromuscular training has shown to decrease their rate of ACL tears. Women also tend to land with their knees in greater extension increasing stress on the ACL. Unfortunately, bracing does not prevent injuries to the ACL. Meniscal tears are also associated with ACL tears. The meniscus helps stabilize the knee. When the ACL is torn, greater stress is placed on it. At five years following an ACL injury without treatment, medial meniscus tears are noted in 25% of reconstructed knees. In 10 years 80% will have torn the meniscus. This is crucial because the meniscus is the major shock absorber of the knee. On the inner side of the knee it transmits 50% of force within the knee in extension and 90% while flexed. Meniscal tears lead to loss of the shock absorber function and predispose the knee to osteoarthritis. Despite accurate reconstruction, mild degrees of arthritis are common in knees after a cruciate ligament tear. As the ACL tear stretches prior to rupture, simply suturing the ligament is ineffective and reconstruction is necessary to return stability to the knee. During ACL reconstruction, bone tunnels are created under arthroscopic control in the anatomic footprint of the ACL in the tibia and femur bones. A graft ,usually hamstring tendon or the central one third patellar tendon, (BTB) is then placed through the bony tunnels and secured with screws and/or other fixation devices.
The diagnosis of an ACL tear is usually made by a clinical test called a Lachman exam which tests the integrity of the ACL. MRI scans confirm the diagnosis and help determine if additional injuries have occurred. Surgery is delayed until the knee has recovered a full range of motion and swelling has diminished. There is a seven times increased risk of scar tissue formation when the ACL is reconstructed within the first three weeks of injury. Generally when range of motion normalizes surgery can be safely performed. Females have two to four times the risk of ACL injuries compared to males. The reasons are not exactly clear, but there seems to be a correlation between ACL tears and the varying phases of the menstrual cycle. Females also have stronger and quicker quadriceps firing in relation to their hamstrings compared to their male counterparts. Preseason training that focuses on proprioceptive conditioning plus neuromuscular training has shown to decrease their rate of ACL tears. Women also tend to land with their knees in greater extension increasing stress on the ACL. Unfortunately, bracing does not prevent injuries to the ACL. Meniscal tears are also associated with ACL tears. The meniscus helps stabilize the knee. When the ACL is torn, greater stress is placed on it. At five years following an ACL injury without treatment, medial meniscus tears are noted in 25% of reconstructed knees. In 10 years 80% will have torn the meniscus. This is crucial because the meniscus is the major shock absorber of the knee. On the inner side of the knee it transmits 50% of force within the knee in extension and 90% while flexed. Meniscal tears lead to loss of the shock absorber function and predispose the knee to osteoarthritis. Despite accurate reconstruction, mild degrees of arthritis are common in knees after a cruciate ligament tear. As the ACL tear stretches prior to rupture, simply suturing the ligament is ineffective and reconstruction is necessary to return stability to the knee. During ACL reconstruction, bone tunnels are created under arthroscopic control in the anatomic footprint of the ACL in the tibia and femur bones. A graft ,usually hamstring tendon or the central one third patellar tendon, (BTB) is then placed through the bony tunnels and secured with screws and/or other fixation devices. 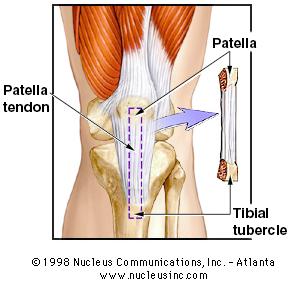 Interestingly it has been clearly determined only in the last few years that the true attachment sites of the ACL have been elucidated. Prior to this the graft was placed at an “isometric “point which has since been shown to yield inferior results and may in fact be a factor contributing to the arthritic changes found in some knees after ACL injuries. The ACL is actually comprised of two bundles, the antermedial and the posterolateral bundles. Most traditional reconstructions observed by Dr. Mead, completely miss the anatomic location of the ACL attachment sites and lead to inferior results.Fortunately, Dr. Mead has been at the forefront of these technological advances that allow for proper graft placement and superior results. Occasionally an athlete will tear only one of the 2 bundles which can still lead to instability. Doctor Mead has the capability of reconstructing both single and both bundle tears. There are several graft choices for ACL reconstruction. The first is the central one third patella tendon with bone from the patella and the tibia remaining attached. This graft has the advantage of secure fixation in the bony tunnels with screws, allowing bone-to-bone healing. Another advantage is that the graph tissue is regenerated at the donor site after the harvest. There is, however, more pain after the surgery due to the donor site morbidity, more difficulty kneeling which can be permanent, and a higher risk of developing arthritis with this graft choice. Quadricep rehab is longer and harder with this graft choice due to the significant atrophy that occurs in the quadriceps secondary to the harvest. This atrophy can be reliably reversed with rehabilitation but it may take up to a year or longer for this to occur. It has been considered the gold standard in the past and still remains an excellent choice for certain athletes.
Interestingly it has been clearly determined only in the last few years that the true attachment sites of the ACL have been elucidated. Prior to this the graft was placed at an “isometric “point which has since been shown to yield inferior results and may in fact be a factor contributing to the arthritic changes found in some knees after ACL injuries. The ACL is actually comprised of two bundles, the antermedial and the posterolateral bundles. Most traditional reconstructions observed by Dr. Mead, completely miss the anatomic location of the ACL attachment sites and lead to inferior results.Fortunately, Dr. Mead has been at the forefront of these technological advances that allow for proper graft placement and superior results. Occasionally an athlete will tear only one of the 2 bundles which can still lead to instability. Doctor Mead has the capability of reconstructing both single and both bundle tears. There are several graft choices for ACL reconstruction. The first is the central one third patella tendon with bone from the patella and the tibia remaining attached. This graft has the advantage of secure fixation in the bony tunnels with screws, allowing bone-to-bone healing. Another advantage is that the graph tissue is regenerated at the donor site after the harvest. There is, however, more pain after the surgery due to the donor site morbidity, more difficulty kneeling which can be permanent, and a higher risk of developing arthritis with this graft choice. Quadricep rehab is longer and harder with this graft choice due to the significant atrophy that occurs in the quadriceps secondary to the harvest. This atrophy can be reliably reversed with rehabilitation but it may take up to a year or longer for this to occur. It has been considered the gold standard in the past and still remains an excellent choice for certain athletes. 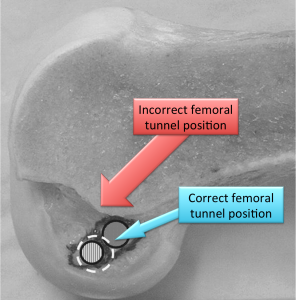 Reconstruction using two of the four hamstring tendons, namely the semi tendinosis and gracilis has become much more popular recently. It’s main limitation in the past was due to difficulty in securing the graft firmly in the tunnels. Newer fixation devices and rehab protocols have largely eliminated this as a concern. There is less pain and leg numbness after harvesting this graft.
Reconstruction using two of the four hamstring tendons, namely the semi tendinosis and gracilis has become much more popular recently. It’s main limitation in the past was due to difficulty in securing the graft firmly in the tunnels. Newer fixation devices and rehab protocols have largely eliminated this as a concern. There is less pain and leg numbness after harvesting this graft. 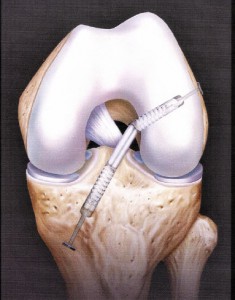 Compared to bone patellar bone autograft there are fewer arthritic changes with time. We can also reconstruct a single bundle with this graft if only one bundle is torn . The tendons do partially regenerate but don’t attach to the normal positions. There is some loss of flexion strength but this is usually not detectable clinically. The rehabilitation is generally much easier with this graft choice. Recently there has been interest in independently reconstructing the two bundles through separate tunnels. At this time there is no clear evidence that outcomes are improved with this double bundle reconstruction compared to well performed anatomic reconstruction. The use of allograft or cadaver tissue is also an option that is appealing because normal anatomy is not sacrificed resulting less pain after surgery.
Compared to bone patellar bone autograft there are fewer arthritic changes with time. We can also reconstruct a single bundle with this graft if only one bundle is torn . The tendons do partially regenerate but don’t attach to the normal positions. There is some loss of flexion strength but this is usually not detectable clinically. The rehabilitation is generally much easier with this graft choice. Recently there has been interest in independently reconstructing the two bundles through separate tunnels. At this time there is no clear evidence that outcomes are improved with this double bundle reconstruction compared to well performed anatomic reconstruction. The use of allograft or cadaver tissue is also an option that is appealing because normal anatomy is not sacrificed resulting less pain after surgery.  There are no rejection concerns but because the tissue is obtained from cadaveric source there is a slight risk of contracting HIV infection or hepatitis. All donor tissue is screened extensively and the grafts processed to minimize the risk of disease transmission. The likelihood of disease transmission is thought to be less than one in 2.5 million. To the best of my knowledge no such infections have occurred since 1985 when HIV testing became available. The main disadvantage to allograft ACL reconstruction is that this graft takes longer to incorporate and undergo transformation to a ligament. Autograft bone patellar bone (BTB) or semi tendinosis/Gracilis (Semi-T/G) incorporate fully by one year after reconstruction. Allograft takes two full years. All grafts actually act as scaffolds – the body repopulates the grafts with the patients own cells that migrate from the bony tunnels. The failure rate of allograft in males less than 23 years old involved in collision sports is 23% at six months but normalizes to a approximately 3% if return to sports is delayed for one year. Athletes with autograft can return to sports at six months. There is no clinical evidence that female athletes with allograft or males in non-contact sports have an increased risk of failure with allograft. In high demand athletes, particularly young male collision athletes, the risk of retear is going to be higher with allograft material.
There are no rejection concerns but because the tissue is obtained from cadaveric source there is a slight risk of contracting HIV infection or hepatitis. All donor tissue is screened extensively and the grafts processed to minimize the risk of disease transmission. The likelihood of disease transmission is thought to be less than one in 2.5 million. To the best of my knowledge no such infections have occurred since 1985 when HIV testing became available. The main disadvantage to allograft ACL reconstruction is that this graft takes longer to incorporate and undergo transformation to a ligament. Autograft bone patellar bone (BTB) or semi tendinosis/Gracilis (Semi-T/G) incorporate fully by one year after reconstruction. Allograft takes two full years. All grafts actually act as scaffolds – the body repopulates the grafts with the patients own cells that migrate from the bony tunnels. The failure rate of allograft in males less than 23 years old involved in collision sports is 23% at six months but normalizes to a approximately 3% if return to sports is delayed for one year. Athletes with autograft can return to sports at six months. There is no clinical evidence that female athletes with allograft or males in non-contact sports have an increased risk of failure with allograft. In high demand athletes, particularly young male collision athletes, the risk of retear is going to be higher with allograft material. 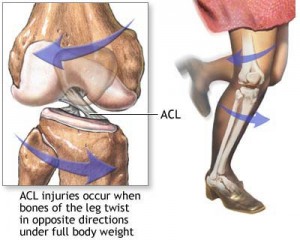 ACL reconstruction is routinely done on an outpatient basis under a general anesthetic. A femoral nerve block can also help control postoperative pain. All surgeries are video recorded and narrated. Physical therapy is begun within several days of surgery. Generally patients are able to fully bear weight immediately after surgery with crutches. Athletes returned to play earlier than six months after reconstruction significantly increase the risk of reinjury.
ACL reconstruction is routinely done on an outpatient basis under a general anesthetic. A femoral nerve block can also help control postoperative pain. All surgeries are video recorded and narrated. Physical therapy is begun within several days of surgery. Generally patients are able to fully bear weight immediately after surgery with crutches. Athletes returned to play earlier than six months after reconstruction significantly increase the risk of reinjury.